Community Acquired Pneumonia (CAP)
Community Acquired Pneumonia (CAP)
Dr Ashraf Mokhtar Madkour, MD, Dr.med., FCCP
Professor Pulmonary Medicine, Ain Shams University
Epidemiology:
Pneumonia remains the seventh leading cause of death in the United States. Estimates of the incidence of community-acquired pneumonia range from 4 million to 5 million cases per year with more than 10 million physician visits and 1.1 million hospitalization in the United States. Mortality reaches 10 to 14% and 30 to 40% in those admitted in ward and ICU respectively.
Pathogenesis:
• Inhalation of infectious particles.
• Aspiration of oropharyngeal or gastric contents.
• Hematogenous deposition.
• Direct inoculation.
• Invasion from infection in contiguous structures
Introduction:
Community-Acquired Pneumonia (CAP) is one of most common infectious diseases and is an important cause of mortality and morbidity worldwide. CAP is as an acute infection of the pulmonary parenchyma in a patient who has acquired the infection in the community, as distinguished from hospital-acquired (nosocomial) pneumonia (HAP). This article will review the up to date management of CAP.
Definitions:
Lower respiratory tract infection An acute illness (present for 21 days or less), usually with cough as the main symptom, and with at least 1 other lower respiratory tract symptom (such as fever , sputum production, breathlessness, wheeze or chest discomfort or pain) and no alternative explanation (such as sinusitis or asthma). Pneumonia, acute bronchitis and exacerbation of chronic obstructive airways disease are included in this definition.
Pneumonia Acute infection or inflammation of the lung parenchyma characterized by clinical & / radiological signs of consolidation of part or parts of one or both lungs.
Community-acquired pneumonia (CAP) refers infection of the lung parenchyma in a person who is not hospitalized or living in a long-term care facility for ≥ 2 weeks. This pneumonia develops in the outpatient setting or within 48 hours of hospital admission
Microbiology:
Many pathogens causes CAP. Table 2 lists the most common causes of CAP, in decreasing order of frequency of occurrence and stratified for severity of illness as judged by site of care (ambulatory vs. hospitalized). Streptococcus pneumoniae remains the most commonly identified pathogen.
|
Age |
Immunocompetent |
Immunocompromised |
External / Behavioral |
|
. > 50 years |
. Cardiovascular/ cerebrovascular disease . Chronic pulmonary disease . Diabetes . Functional / anatomical asplenia . Alcoholism . Alcoholism . Chronic liver disease . Cerebrospinal fluid leaks |
. HIV . Chronic renal failure / nephrotic syndrome . Cancer (solid, hematologic) . Organ / bone marrow transplant . Autoimmune diseases . Immunosuppressive therapy / corticosteroids . Primary immunodeficiencies |
. Smoking history . Heavy alcohol use . Recent viral respiratory infection |
Factors that increase risk for development of CAP
The clinical diagnosis of CAP:
All patients should have full medical history and physical examination and exclude conditions that can mimic pneumonia.
Symptoms:
May be preceded by upper respiratory tract infection. Respiratory symptoms: Cough dry or productive, mucopurulent sputum , sometimes rusty, dyspnea, sometimes pleuritic chest pain. Non-respiratory symptoms: Fever, bodyaches, altered mental state, vomiting or diarrhea.
Signs:
Generally: Fever, sometimes hypothermia, tachycardia, tachypnea. Local: signs of consolidation.
Diagnosis
is based on suggestive clinical features, new infiltrate in chest x-ray (or other imaging) with or without supporting microbiological data.
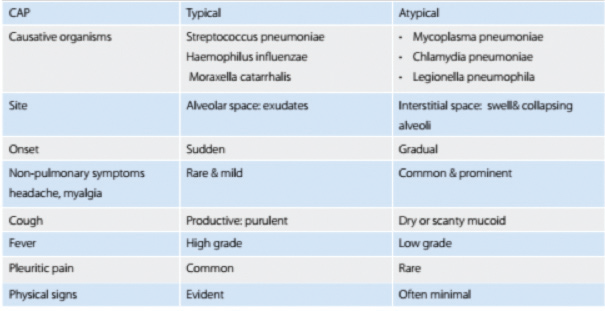
Typical and atypical bacterial pathogens may have different clinical presentations of CAP.
|
Patient type |
Etiology |
|
Outpatient |
Streptococcus pneumonia Mycoplasma pneumonia Haemophilus infl enzae Chlamydophila pneumonia Respiratory viruses |
|
Inpatient (non – ICU) |
S. pneumonia M. pneumonia C. pneumonia H. influenza Legionella species Aspiration Respiratory viruses |
|
Inpatient (ICU) |
S. pneumonia Staphylococcus aureus Legionella species Gram-negative bacilli H. influenzae |
Radiological diagnosis of CAP:
“No diagnosis of pneumonia without at least chest x-ray”
The value of Chest x-ray in CAP is to establish the diagnosis, evaluate the severity (e.g. multilobar or bilateral disease may indicate severe pneumonia), identify co-existing conditions (e.g. bronchial obstruction or abscess) and identify pattern of infiltrates. CT scan may assist in the diagnosis of CAP severity and help in differential diagnosis.
Diagnostic testing:
Recommendations for diagnostic testing remain controversial in CAP. It is optional in outpatient setting while it is mandatory in all critically ill CAP and when specific pathogen is suspected.
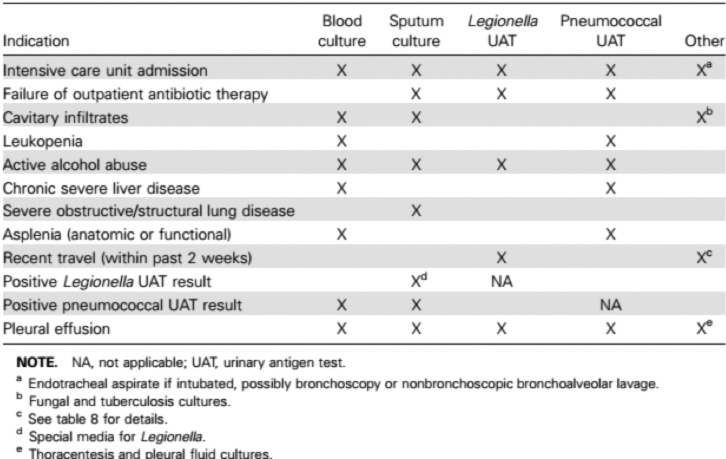
Diagnostic testing for CAP etiology may include: sputum gram stain, sputum culture and sensitivity, sputum for acid fast bacilli by Ziehl–Neelsen stain, blood culture, acute phase serologic testing (e.g. Chlamydophila, Mycoplasma & Legionella), urinary antigen testing (e.g. Legionella and Pneumococcal) and PCR.
Other diagnostic testing for CAP may be indicated in special situations may include: Bronchoscopic bronchoalveolar lavage, endotracheal tube aspirate, thoracocentesis and transthoracic needle aspiration biopsy.
The clinical indications for more diagnostic testing are shown in table 4
Site of Care
Decisions &
Severity of CAP:
Assess the severity of pneumonia and site of receiving care through an objective tool for risk assessment using CURB 65 scoring system for pneumonia which consists of 5 risk factors each scores one point, for a maximum score of 5.
CURB 65 scoring system for pneumonia:
• Confusion.
• Blood urea nitrogen > 19 mg per dL.
• Respiratory rate ≥ 30 breaths per minute.
• Systolic blood pressure < 90 mm Hg or Diastolic blood pressure ≤60 mm Hg.
• Age: ≥ 65 Years.
Patients are stratified for risk of death as follows:
• CURB65 score 0 or 1: low risk (less than 3% mortality risk)
• CURB65 score 2: intermediate risk (315%- mortality risk)
• CURB65 score 3 to 5: high risk (more than 15% mortality risk).
Use clinical judgement in conjunction with the CURB65 score to guide the management of community-acquired pneumonia, as follows:
• consider home-based care for patients with a CURB65 score of 0 or 1
• consider hospital-based care for patients with a CURB65 score of 2 or more
• consider intensive care assessment for patients with a CURB65 score of 3 or more.
Treatment:
All treatment detailed here are based on The official Statement of the Egyptian Scientific Society of Bronchology (ESSB), May 2012 on the Management of Adult Lower Respiratory Tract Infections A Consensus Statement
1. General Recommendations:
1.1- Empirical Treatment is recommended
• The start of empirical treatment should not be delayed.
• An “Appropriate” empirical treatment refers to the use of an antibiotic to which the possible etiological microorganism(s) are sensitive. “Adequate” treatment refers to the use of an appropriate antibiotic at the correct dosage, with good penetration at the site of the infection and, when indicated, in a combination.
• In selecting empiric therapy for patients who have recently received an antibiotic, an effort should be made to use an agent from a different antibiotic class.
• Factors taken in consideration before selection of empirical antibiotic therapy:
- Antibiotic taken in last 3 months.
- Ask about the history of sensitivity to any antibiotic.
-Underlying co-morbidity to avoid or adjust dose e.g. renal impairment, liver impairment …etc.
1.2- Where to treat the patient with CAP:
• Most patients with CAP can be treated at home.
• Those who fail to improve after 48 h of treatment should be considered for hospital admission or revise diagnosis.
• Patients admitted in hospital or ICU according to assessment using CURB 65 scoring system as described before.
1.3- General management strategy for patients treated in the community
- Patients with suspected CAP should be advised to rest, to drink plenty of fluids and not to smoke.
- Patients diagnosed with CAP should be isolated and take precautions of infection control.
- Pleuritic pain & Fever should be relieved using simple analgesia such as paracetamol.
2. Recommendations for the Empirical Treatment: Outpatient treatment:
Oral Respiratory Fluroquinolones
Or Oral B-Lactam/ B-Lactamase + Oral New Macrolide
Or IM 3rd Generation Cefalosporines + New Macrolide
• In-patient treatment: Non-ICU:
Intravenous (ⅠV ) Respiratory fluoroquinolone
Or ⅠV B-Lactam/ B-Lactamase + ⅠV New Macrolide
Or ⅠV 3rd Generation Cephalosporin + ⅠV New Macrolide
• In-patient treatment: ICU: No Monotherapy.
ⅠV Respiratory fluoroquinolone + 3rd or 4th generation cephalosporin Or ⅠV Imipenem + ⅠV New Macrolide
• Special entities in ICU:
- Aspiration:
As Before +ⅠV. Clindamycin Or Metronidazole
- Risk of Pseudomonas Infection:
Antipseudomonal beta-lactam (3rd or 4th generation cephalosporin Or Piperacillin-tazobactam Or carbapenem)
Plus (aminoglycoside Or antipseudomonal fluoroquinolone)
-For community-acquired methicillin-resistant Staphylococcus aureus infection (MRSA):
Add Teicoplanin Or linezolid
Alternative: Vancomycin (considering its renal side effects)
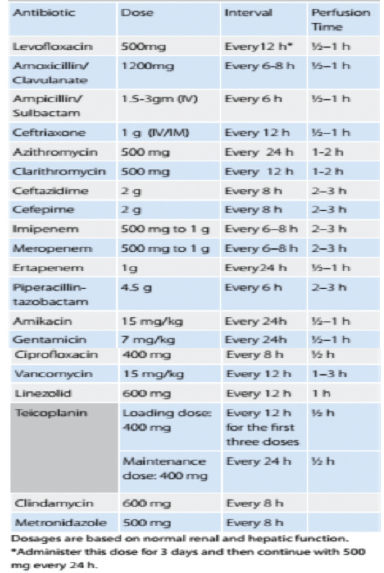
Recommended adult doses and intervals for the main antibiotics recommended in the treatment for CAP are shown in table 5 & 6
|
Group |
Antibiotic |
Dose |
Interval |
|
Respiratory Fluoroquinolone |
Levofloxacin Gemifloxacin Moxifloxacin |
750 mg 320 mg 400 mg |
Every 24 h Every 24 h Every 24 h |
|
ß - Lactam / ß - Lactamas |
Amoxicillin/ Clavulanate |
1 g |
Every 8-12 h |
|
New Macrolide |
Azithromycin Clarithromycin |
500 mg 500 mg |
Every 24 h Every 12 h |
3. Switching from intravenous to oral:
• Patients treated initially with parenteral antibiotics should be transferred to an oral regimen when they are hemodynamically stable and improving clinically, are able to ingest medications, and have a normally functioning gastrointestinal tract.
• Patients should be discharged as soon as they are clinically stable (Criteria for clinical stability: temperature ≤37.8°C, heart rate ≤100 beats/min, respiratory rate ≤24 breaths/min, systolic blood pressure ≥90 mm Hg, arterial oxygen saturation ≥90% or pO2 ≥60 mm Hg on room air, ability to maintain oral intake and normal mental status), have no other active medical problems, and have a safe environment for continued care. Inpatient observation while receiving oral therapy is not necessary.
4.Duration of the Treatment:
•Patients with CAP should be treated for a minimum of 5 days, should be afebrile for 48–72 h, and should have no more than 1 CAP-associated sign of clinical instability before discontinuation of therapy.
For patients managed in the community and for most patients admitted to hospital with low or moderate severity and uncomplicated pneumonia, 7 days of appropriate antibiotics is recommended. For those with high severity microbiologically-undefined pneumonia, 7–10 days of treatment is proposed.
• A longer duration of therapy may be needed if initial therapy was not active against the identified pathogen or if it was complicated by extrapulmonary infection.
Considerations for patients worsening or failing to improve by day three:
• Predisposing condition requiring >3 days for improvement (continue present treatment) e.g. elderly patient
• Incorrect diagnosis or complicating condition
• Common: Pulmonary embolism or infarction, carcinoma, pulmonary edema, bronchiectasis, etc.
• Uncommon: Pulmonary eosinophilia, alveolar hemorrhage, foreign body
• Unexpected pathogens: e.g. mycobacteria, MRSA etc.
Prevention and vaccination:
1. Influenza and pneumococcal vaccination
The prevention of CAP, particularly in those considered at high risk of infection, is an important issue in the overall management. All patients aged 65 years or at risk of invasive pneumococcal disease who are admitted with CAP and who have not previously received pneumococcal vaccine should receive 23-valent pneumococcal polysaccharide vaccine (23-PPV). Influenza vaccine should be offered to persons at hospital discharge or during outpatient treatment during the fall and winter.
2. Smoking cessation
Cigarette smoking, both active and passive, is a recognized independent risk factor for CAP. Smoking cessation should be a goal for persons hospitalized with CAP who smoke


 info@utopiapharma.com
info@utopiapharma.com
 Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia
Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia