Choice of Antibiotics in Management of Lower Respiratory Tract Infections
Choice of Antibiotics in Management of Lower Respiratory Tract Infections
Dr. Adel Khattab , MD , FCCP Professor of Pulmonary Medicine , Ain Shams University
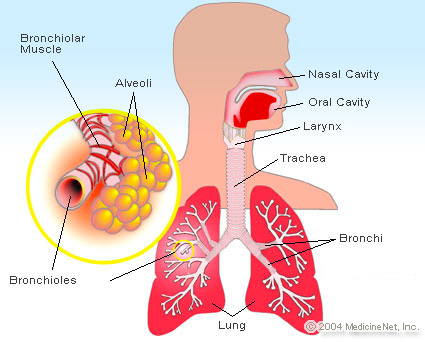
Acute lower respiratory tract infections (LRTIs ) are a leading cause of death worldwide. In USA , LRTIs are the most common cause for antibiotic prescription inside the hospitals. The great problem is that , by the end of the 20th century , the antibiotics are no longer effective against killing bugs , this is mainly due to increase bacterial resistance. Many issues to be considered in antibiotic choice : - Bacterial resistance. - Patient compliance. - PK / PD. - Eradication of bacteria.
Bacterial Resistance
There is emerging and increasing resistance of different bacteria against most of the available antibiotics. For example , Strept. Pneumonia which is the most common causative pathogens in LRTIs. In the early 1960s , the first report of strains resistant to penicillin. In the new millennium , resistance is increasing worldwide primarily against beta lactams and macrolides. In Egypt , according to multicentres study in 2013 , Strept. Pneumonia resistance to ampicillin is 32 % , Clindamycin 51 % , Co- trimoxazole 63 %. 1st generation Cephalosporins 32 % , 3rd generation cephalosporins 21 % , gentamycin 72 % and Ciprofloxacin 21 %. There is also increasing beta lactamase producing strains in the Haemophilis influenza and Morexalla catarrahlis. For control of antibiotic resistance inside the hospitals , it requires aggressive implementation of several strategies - Ongoing surveillance of resistance. - Use hygienic control to limit spread of strains.- - Use closed formularies for prescription of antibiotics to limit prescribing options to one or two drugs per class. Restriction of the use of antibiotics.- - Rotational use of antibiotics (Antibiotic Cycling Program).
Patient Compliance and Bacterial Resistance
Patient who skip a dose and do not complete the regimen are unlikely achieving optimum antibiotic concentrations , that is closely linked with bacterial resistance. Therefore , non compliance with an antibiotic may lead to selection of bacterial resistance. Non – compliance is directly related to length of treatment and daily doses. So , WHO recommendations support the prescribing of the potent antimicrobial that has a shorter period of time , in order to minimize the risk of resistance development
Pharmacokinetics & Pharmacodynamics of Antibiotics
The potency of antibiotic is the product of both antibacterial
activity and the ability to deliver antimicrobial agents to the
site of infection in sufficient concentrations to eradicate
the microorganisms. Pharmacokinetics means what the
body will do with the antibiotic starting by absorption , metabolism ,
distribution and elimination. While pharmacodynamics means what
the antibiotics will do inside the body ( how it will kill the bacteria) ,
according to tissue concentration or the time the antibiotic will be on
the tissue with sufficient concentration. So , antibiotics are divided
into :
1-Concentration –dependent antibiotics :
Aminoglycosides , Quinolons.
2-Time – dependent antibiotics :
B-lactams , Macrolides and Clindamycin.
3-Time –dependent with post antibiotic effect :
Azithromycin , tetracyclin.
The most important concentration , is not serum concentration or
tissue concentration but concentration at the site of infection :
A- Antibiotics with good penetration into the sputum , bronchial
secretions and bronchial mucosa : New macrolides , ketolides ,
quinolons ,tetracyclin , co – trimoxazole and clindamycin.
B- Antibiotics with poor penetration into the sputum :
aminoglycosides and B- lactams.
If you use the appropriate antibiotic , this will lead to bacterial
eradication with maximization of the clinical response and
minimization of bacterial resistance. While inappropriate
treatment leads to failure of bacterial eradication and selection
of resistant bacteria. So , the goal of the antibacterial therapy is to
eradicate common bacteria from the site of infection.
General recommendation in the use of antibiotics
3-The start of empirical treatment should not be delayed due to the
need for performing diagnostic sampling microbiological studies.
2-Use appropriate antibiotic which means the possible organisms are
sensitive.
3-Treatment should be adequate which means , appropriate antibiotic
at the correct dosage with good penetration at the site of infection
and , when indicated , in good combination.


 info@utopiapharma.com
info@utopiapharma.com
 Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia
Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia