Appropriate Antibiotic Use For Acute Rhinosinusitis
Mamduoh El-Gohary Prof.of.Oto Laryngology Ain Shams University
Appropriate Antibiotic Use For Acute Rhinosinusitis
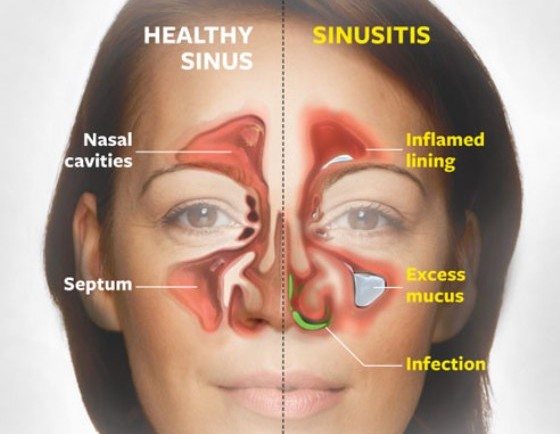
The term sinusitis refers to inflammation of the mucosa of the paranasal sinuses. Because sinusitis is invariably accompanied by inflammation of the contiguous nasal mucosa, rhinosinusitis has become the preferred term.Acute rhinosinusitis is frequently caused by viral infection.
It will often resolve in most patients without antibiotic treatment. Acute rhinosinusitis is defined by symptom duration of less than 4 weeks Acute bacterial sinusitis is usually a secondary infection resulting from sinus ostia obstruction, impaired mucus clearance mechanisms caused by an acute viral upper respiratory tract infection, or both.
The gold standard for diagnosis of bacterial sinusitis is sinus puncture,and streptococcus pneumoniae and Haemophilus influenzae are the bacteria most commonly isolated from infected maxillary sinuses.
Streptococcus pyogenes, Moraxella catarrhalis and small percentage of each account for an aerobicbacteria bacterial sinus infection However, sinus puncture is an invasive procedure, seldom performed in primary care.
Because no simple and accurate office-base tests for acute bacterial rhinosinusitis are available clinicians rely on clinical findings to make the diagnosis. However, signs and symptoms of acute bacterial rhinosinusitis and of prolonged viral upper respiratory tract infections, are similar, making the clinical diagnosis of acute bacterial rhinosinusitis difficult and resulting in frequent misclassification of viral cases.
The clinical diagnosis of acute bacterial rhinosinusitis should be reserved for patients with rhinosonusitis symptoms lasting 7days or more who have maxillary pain or tenderness in the face or teeth especially when unilateral and purulent nasal secretions.
TREATMENT
Acute bacterial rhinosinusitis resolves without antibiotic treatment in most cases. symptomatic treatment is the preferred initial management strategy for patients with mild symptoms Antibiotic therapy shouuld be reserved for patients with moderate to severe, symptoms. In most cases, only patients with the specific findings of maxillary pain or tenderness in the face or teeth and persistent purulent nasal discharge who are not improving after 7 days and those with severe symptoms, regardless of duration, should be treated with antibiotics.
Antimicrobial selection in acute Bacterial Rhinosinusitis(ABRS) Antimicrobial classes include B-lactams, fluoroquinolones macro- lides, Azalides, lincosamides, tetracyclines, and sulfonamides/ trimethoprim B- lactams: the B-lactam class of antimicroboals includes a broad range of compounds with significantly different spectra of activity.
These agents all share a common, sructural component : the B-lactam ring orally available agents include the penicillins and the cephalosporins.
1- Amoxicillin(Amoxil) Amoxicillin is relatively safe and well tolerated.Activity is limited by its destruction by the B-lactamases produced by some strains of H-influenzae, M. catarrhalis, stahylococcus, and gram negative oral anaeorbic species. Amoxicillin is generally considered the most active of all the oral B- lactams against streptococci, including pneumococci. Resistance to penicillin in isolates of S. pneumoniae is relative and may be overcome in most cases by using higher doses of amoxicillin. Although the typical adult amoxicillin dose is 1.5 - 1.75gm /day 2-3 times higher daily doses may be necessarys to eradicate isolates of s. pneumonia.High-dose amoxicillin has not been approved by the FDA or systematically evaluated and its safety profile is not yet well defined. The intrinsic activity of amoxicillin against B-lactamase negative strains of H. influenzae is fair to. good However, amoxicillin is ineffective against B-lactamase producing strains.
2- Amoxicillin /clavulanate (Augmentin) Clavulanate enhances amoxicillins It activity against B- lactamase producing strains of H- influenzae, M.catarrhalis, staph. and oral anaerobes. When given as a 3 times / day regimen, it has been associated with a high incidence of gastro intestinal side effects.This problem has significantly decreased with twice a day dosing.
3- Cefuroxime axetil(Ceftin) has a good potency, efficacy and side - effect profile. It has limited activity against s. pneumoniae. It is effective against most of strains H.influenzae
4- Cefpodoxime proxetil(Vantin) it has potent activity against H.influenzae strains and comparable activity to ceftin against s.pneumoniae
5- Cofprozil (Cefzil) It has activity against pneumococcus that is comparable to ceftin and vantin. However, it has markedly less activity against H.influenzae
6- Cefixime(Suprax) It has a potent activity against H. influenzae but provides weak gram -positive coverage including s. pneumoniae.It has no activity against staph.
7- Cefaclor(Ceclor) it has poor activity against H. influenzae fair against penicillin susceptible pneumococci.therefore cefaclor has poor overall efficacy against bacterial respiratory tract pathogens
II-Fluoroquinolones: Gatefloxacin(Tequin) , levofloxacin(Levoquin), and moifloxacin(Avelox).
These newer fluoroquinolones have remarkable potency against H.influenzae and M .catarrhalis and unlike ciprofloxacillin, strong potency against s. pneumoniae They generally lack the phototoxicity seen in other quinolones. The fluoroquinolones are currently not approved for use in children
III-Macrolides / Azolides Erythromycin, clarithromycin and azithromycin (Zithromax) .These agents have activity against gram - positive and some gram - negative bacteria. All the macrolides have good activity against macrolide susceptible pneumococci However, the increasing rate of macrolide resistance to s. pneumoniae is associated with a significant likelihood of clinical failure. Although clarithromycin and azithromycin have slightly greater activity against H influenzae than erythromycin most of the available eradication and efficacy studies suggest an activity that is similar to or marginally higher than that of placebo.
IV- Lincosamides Clindamycin is the primary lincosamide antibiotic in clinical use It is used for the treatment of susceptible gram-positive aerobes and anaerobes as well as many gram-negative anacrubes. it is not,However, active against H.influenzae or M. catarrhalis.
V-Tetracyclines. Doxy Cycline(Vibramycin) It has adequate activity against penicillin susceptible pneumococci. It has activity against M. catarrhalis but its activity against H. influenzae is limited by its pharmacokinetics clinicians should be aware of the possibility of photosensitivity and infrequent esophageal caustic burns Like the other tetracyclines, usage in children younger than 8 years is contraindicated because of the possibility of tooth enamel discoloration.
Vi- Sulfonamides And Trimethoprim High rates of resistance to thes drugs is now present in pneumocci and H. influenzae. M. ctarrhalis is intrinsically resistant to sulfamethoxazole. In addition, these agents are more likely to cause skin rash, erythema multiforme and toxic epidermal, necrolysis which can be potentially fatal. Antimicrobial: Treatment guidelines: Initial antibiotic treatment should be with narrow spectrum agents On the basis of clinical trials amoxicillin /clavulanate, Amoxicillin, cefpodoxime poxetil, cefuroxime axetil are the favored antibiotocs. In case of Beta lactam allergic patients, Azithromycin, clarithromycin, erythromycin, clindamycin are used. If no improvement or worsening of symptoms after 72 hours occurs switch therapy options include Fluoroquinolones and reevaluation of patients.


 info@utopiapharma.com
info@utopiapharma.com
 Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia
Plot No. (2) Industrial Zone (A7) - formerly Zizinia - Cairo - Ismailia Road - 10th of Ramadan - Sharkia